
About Monkeypox
Monkeypox is a rare viral infection mainly spread by wild animals. It is generally very rare in Europe.
Initial symptoms of monkeypox include fever, headache, muscle aches, backache, swollen glands, chills and exhaustion. New unexpected or unusual spots, ulcers and blisters can develop anywhere on the body, including the face, and other parts of the body including the hands, pubis and genitals (penis, testicles, vulva, front hole and anus). In many cases only one or a few spots or ulcers are being found.
Situation in Spain
In Spain, according to data from the National Epidemiological Surveillance Network (RENAVE), as of October 25 a total of 7,317 confirmed cases of MPX have been reported.
The reported cases come from 17 Autonomous Communities.
Of the cases reported, a total of 7,159 are men and 158 are women. The age ranges from 7
months and 88 years, with a median age of 37 years.
What to do if you think you have symptoms or are a close contact.
In case of any symptoms you should contact your family doctor or call on 900112061 and remain in self-isolation until any suspicion has been discounted, especially if you’ve been a close contact of someone with a positive diagnosis. Avoid attending any events, having close contact with anyone and travel.



FAQs
What is Monkeypox?
Monkeypox is an illness caused by the monkeypox virus. It is a viral zoonotic infection, meaning that it can spread from animals to humans. It can also spread from humans to other humans and from the environment to humans.
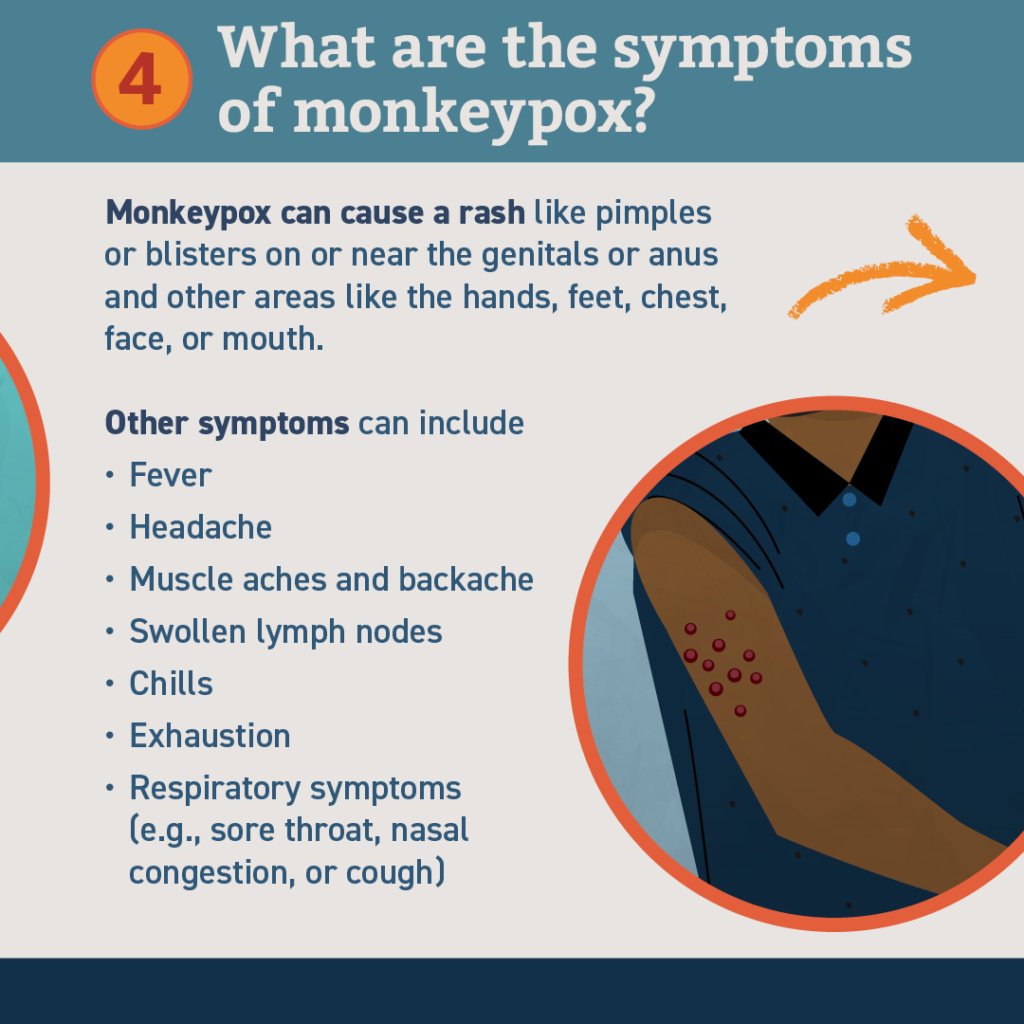
What are the symptoms of monkeypox?
Monkeypox can cause a range of signs and symptoms. While some people have less severe symptoms, others may develop more serious illness and need care in a health facility. Those typically at higher risk include people who are pregnant, children and persons that are immunocompromised.
The most common symptoms of monkeypox identified during the 2022 outbreak include fever, headache, muscle aches, back pain, low energy and swollen lymph nodes, followed or accompanied by the development of a rash which may last for two to three weeks. The rash can affect the face, palms of the hands, soles of the feet, groin, genital and/or anal regions. It may also be found in the mouth, throat, anus or vagina, or on the eyes. The number of sores can range from one to several thousand. Sores on the skin begin flat, then fill with liquid before they crust over, dry up and fall off, with a fresh layer of skin forming underneath.
There are ongoing studies to keep track of and better understand symptoms during this new outbreak, including what parts of the body can be affected and how long symptoms may last.
Anyone who has symptoms that could be monkeypox or who has been in contact with someone who has monkeypox should call or visit a health care provider and seek their advice.
Symptoms usually go away on their own or with supportive care, such as medication for pain or fever. People remain infectious until all of the sores have crusted over, the scabs have fallen off and a new layer of skin has formed underneath.
How is Monkeypox transmitted?
Monkeypox does not spread easily between people. However, it can be caught from:
- touching clothing, bedding or towels used by someone with the monkeypox rash,
- touching monkeypox skin blisters or scabs,
- the coughs or sneezes of a person with the monkeypox rash.
We’re learning more from the latest cases, and while it is not thought monkeypox can be sexually transmitted, close contact during sexual activity can lead to transmission. This could include if your face, lips, hands or fingers (or other skin to skin contact during sex) comes into contact with monkeypox rash or lesions from having sex on their bedding or from respiratory fluids exchanged during kissing, oral sex or sneezing.
Do condoms prevent you catching or passing on monkeypox?
We always encourage use of condoms to prevent sexually transmitted infections (STIs). Monkeypox is not an STI by nature, though it can be passed on by direct contact during sex.
The spots, ulcers and blisters, which are most likely to pass on monkeypox, can appear on any part of the body, so condoms will not necessarily prevent transmission of the virus between two people who are in direct contact, including during sex.
Although it is not clear if monkeypox can be transmitted through genital secretions, some are advising the precaution of using condoms for 12 weeks after all spots or ulcers have cleared.
Monkeypox can also be passed on through contact with clothing, bedding and towels used by someone with monkeypox.
What can I do to reduce the risk of catching monkeypox?
Although monkeypox is rare, there are things you can do to reduce your risk of getting it.
This information is being reviewed carefully as we learn more about the latest cases identified in gay and bisexual men.
- Do not share bedding or towels with people who are unwell and may have monkeypox.
- Do not have close contact with people who are unwell or have symptoms of monkeypox.
- You should wash your hands with soap and water regularly or use an alcohol-based hand sanitiser as you may have come into contact with skin lesions or secretions which might have ended up on your hands.
Can monkeypox be treated?
Treatment for monkeypox aims to relieve symptoms. The illness is usually mild and most people recover in two to four weeks.
People with likely or confirmed monkeypox can isolate at home until they have recovered if they are well enough and able to self-isloate. A small number of people may need to stay in a specialist hospital, so the symptoms can be treated.
Most people with monkeypox recover within a few weeks. There is advice for people who recover to use condoms during sex for up to 12 weeks after they were exposed to monkeypox in Gran Canaria. However, it is important to remember that you can still pass it on through skin to skin contact whilst you have a monkeypox rash, or spots, ulcers and blisters.
Does monkeypox affect PrEP effectiveness?
No. PrEP (pre-exposure prophylaxis) is still effective. People who use PrEP should continue to take it.
Image by Alexandra_Koch from Pixabay




