
We point you to the library “infoVIHtal” of the charity, gTt-VIH, the Working Group for HIV Treatments.
Here you will find all the information you might need on HIV and other STIs.

If you want us to help you change something in your consumption or in your sexuality or give you strategies to reduce risks when consuming, we have agreed to refer you to Yrichen, Fundación Canaria and their support service to offer you an anonymous, confidential, free, respectful of experience of your sexuality and your consumption of drugs or other substances.
It is not necessary to stop using nor is it necessarily the goal. The goal is set by you.
It is run by professionals from the gay community (psychologists, mediators and social workers).
Psychological care: a team of psychologists who will offer you support, guidance and will propose a therapeutic process based on your needs and the objectives set.
Social care: a social worker will offer you information, follow-up, referral and accompaniment to the Drug Dependency Care Network or other socio-health resources. Also information and management of the health card and registration.
Advice on reducing harm and risks in your consumption to help you avoid unwanted consequences.
If you need more information, please contact us at chemsex@yrichen.org
Locations and Telephones:
Addictions Unit, Telde
Calle Sor Carmen Peña Pulido s/n Telde, La Pardilla
Contact Numbers: 828 025 419 / 621 249 559
Addictions Unit, San Bartolomé de Tirajana
Calle Uruguay Nº 5 El Tablero.
Contact Numbers: 928 723 400 (ext 1680) / 652 082 205
We currently conduct HIV and Hepatitis-C tests along with Hepatitis-B, Syphilis, Chlamydia and Gonorrhoea or general sexual health consultations.
Here’s what you can expect during the STI testing:
Our STI testing appointments fill up quickly. If you see no appointments available, please check back again soon. This means that we are fully booked for the next 2 weeks approx. We aim to open the calendar for each month in the last week of the previous month.
We are contributing to a study of the “chemSex” phenomenon convened by the Fundación Canaria Yrichen.
The consultants are requesting the participation of our collective.
Are you the owner of a leisure site or sex venue? Are you a “chems” user or do you practice chemsex? Do you have opinions on the subject, or experience of chemsex parties or chills being a user or not?
You can get involved anonymously by questionnaire or by videoconference or phone call, preferably in Spanish but no one is excluded. checkpoint can act as an intermediary to maintain anonymity or we can put you in direct contact.
Send us an email: chemsex@checkpointcanarias.com or call us: 828 6 43210.
The innovative therapy is long acting and consists of two medications, cabotegravir and rilpivirina.

STIs (sexually transmitted infections) are an extensive group of infections that, as their name indicates, are transmitted from person to person during sexual intercourse.
They are caused by different types of microbes such as viruses, bacteria and protozoa. They mainly affect the genital organs although they can also localise in other parts of the body such as the mouth and the anus.
There are STIs that even invade the bloodstream and lymphatic system. They can affect different vital organs and have serious consequences if they are not treated, as well as significantly increase the risk of being infected by HIV.
They are mainly transmitted during sexual intercourse without a condom, orally, anally and vaginally. Some STIs are only transmitted when there is an exchange of body fluids such as semen, urethral secretions or blood from an infected person (HIV, Hepatitis B and C). Others on the other hand are simply transmitted through direct contact with areas of the skin or mucosal tissue affected by the infections (syphilis, gonorrhea, chlamydia, genital herpes and genital warts).
Did you know that you can have an STI even though you don’t have any symptoms?
It is important to detect them and treat them promptly.
Chlamydia is a sexually transmitted infection (STI) that is transmitted through anal and vaginal penetration and oral sex. It is one of the most frequent STIs, along with syphilis and gonorrhea.
Chlamydia can cause irreversible lesions to the sexual organs and cause infertility. You should take into account that chlamydia and many other STIs can increase the chances of being infected with HIV.
Even so, 50% of chlamydia infections do not present with any symptoms. That’s why many people do not know that they have it and since they don’t seek treatment they continue to pass it on to their partners.
If you suspect that you may have chlamydia you should go to a healthcare centre and they will give you the necessary tests. If the results come out positive you will be prescribed treatment. You need to notify your sexual partners and refrain from sex until you are cured.
Chlamydia is cured with antibiotics such as azithromycin or doxycyline.
It is a chronic infection caused by Chlamydia trachomatis, which affects the genitalia and the inguinal lymph nodes. One of the ways it is transmitted is through anal sex.
If it is treated the prognosis is good, but if left untreated complications may appear years later.
If you suspect that you may have lymphogranuloma (LGV) go to a healthcare centre where you will be given a test to see whether you have the infection.
The infection can be treated with an extended course of the right antibiotics. Among those most commonly prescribed to treat LGV are doxycycline and erythromycin.
Gonorrhea is a sexually transmitted infection (STI) that is caught through anal and vaginal penetration and oral sex. It is one of the most frequent STIs along with syphilis and chlamydia.
Gonorrhea can cause permanent lesions to the sexual organs and lead to infertility. It can also cause pain and swelling in the knees and other joints, small red blisters on the skin and heart problems. You should take into account that gonorrhea and many other STIs can increase the chances of getting infected with HIV.
However, in many cases gonorrhea does not present with any symptoms. That’s why many people do not know they have it and since they don’t get treated they continue to pass it on to their partners.
If you suspect that you may have gonorrhea you should go to a healthcare centre and they will give you the necessary tests.
Gonorrhea is cured with antibiotics. There is an increasing resistance to antibiotics and treatment options are limited.
Syphilis is a sexually transmitted infection (STI) that is caught through anal and vaginal penetration and oral sex, and even through skin contact with a syphilitic lesion. It is one of the most frequent STIs along with gonorrhea and chlamydia.
If not properly treated, years later syphilis can cause serious mental, mobility, sight and heart disorders. You should take into account that syphilis and many other STIs can increase the chances of getting infected with HIV.
However in many cases syphilis does not present with any symptoms or they may gradually go away although the infection persists. That’s why many people do not know they have it and since they don’t get treated they continue to pass it on to their partners.
If you suspect you may have syphilis you can arrange an appointment at BCN Checkpoint to get tested for it. It is a rapid test that will tell you whether you are infected with syphilis in 20 minutes by just drawing a few drops of blood.
Syphilis is cured with antibiotics, typically a single large dose of a penicillin or an extended course of doxycycline. Length and type of treatment will depend on the suspected duration of infection.
The human immunodeficiency virus (HIV) can be transmitted through sexual intercourse: by anal and vaginal penetration and, more rarely, through oral sex.
HIV infection weakens the immune system and if it is not treated over the years it leads to AIDS which brings on a series of diseases that may cause death.
HIV is usually an asymptomatic infection although when the virus enters the body it may cause the following symptoms which often go unnoticed:
Even though these symptoms clear up spontaneously, if it is not treated the infection progresses and weakens the immune system until the person ends up developing AIDS.
If you suspect that you may have HIV ask for an appointment to take the test. It is a rapid test that only requires a few drops of blood and in only 20 minutes you will know whether you are infected with HIV. At the same time you will receive counselling on sexual health and, in the event the result comes out positive, all the psychological support you need.
Hepatitis A is an infection of the liver caused by a virus. One of the ways it is spread is through oral-anal contact given that the virus is present in faeces.
The majority of people who contract hepatitis A recover completely and once they have been through it they cannot get it again. Some people may become seriously ill and may need to be hospitalised.
The symptoms appear 2 to 7 weeks after catching the virus and can last anywhere from 2 weeks to 6 months although some adults do not have any symptoms.
If you suspect that you have hepatitis A you should go to a healthcare centre where you will be given a blood test that will tell you whether you have had the infection.
People with hepatitis A need to rest and follow a healthy diet to ensure that the symptoms gradually subside. It is also very important for a person who is recovering from hepatitis A to abstain from drinking alcohol because it is very difficult for the liver to eliminate it from the body.
There is no cure for hepatitis A but there is a vaccine that protects you from the virus that causes it. BCN Checkpoint runs a free vaccination programme for both hepatitis A and hepatitis B.
Hepatitis B is an infection of the liver caused by a virus. In sexual contact it can be transmitted through anal and vaginal penetration without a condom, and to a lesser extent through oral sex.
Most people who are infected with Hepatitis B recover completely but in some cases it may become chronic, producing hepatic lesions which in some cases could cause liver cancer and even lead to death.
However, some hepatitis B infections do not present with any symptoms. This means that many people do not know that they have it and since they don’t get treated they continue to transmit it to their partners.
If you suspect that you may have hepatitis B go to a healthcare centre where you can take a blood test that will tell you whether you have or have had hepatitis B.
There is no cure for hepatitis B. However there is a vaccine that can protect you from the virus that causes it. Certain antirretroviral can also be used to control the infection.
Hepatitis C is a liver infection caused by a virus. It is basically spread through blood contact with an infected person and consequently, sex where there might be contact with blood entails a higher risk of transmission.
Lately there has been an increase in the number of cases of hepatitis C infections through sex in gay men, associated with practices such as penetration without a condom, group sex, sharing sex toys and fisting without protection, which may produce small lesions.
It may become dangerous. With time people who have chronic hepatitis C run the risk of developing serious health problems such as:
The effects of hepatitis C may take years to manifest themselves. In some cases serious symptoms do not appear until 30 years later.
If you have any of these symptoms and they do not go away after a few days go to a healthcare centre. If you have jaundice go immediately.
If you suspect that you might have hepatitis C you can take a blood test to find out whether you have been infected.
New drugs have come out recently which can cure hepatitis C although they are only administered for very serious cases.
Genital warts appear as a small bump or group of bumps in the genital area and are normally painless. They are acquired through anal and vaginal penetration, through contact between the skin and a wart and through oral sex.
Genital warts are caused by the human papilloma virus (HPV), a virus that is very easily transmitted. In the majority of cases it does not cause any symptoms or health problems to people infected with it.
Genital warts are caused by a less serious HPV type and are not usually associated with cancer. There is another more serious type of HPV virus that does not produce warts or any other apparent symptoms and that can increase your risk of anal cancer.
External warts can sometimes be clearly visible. Internal ones need to be diagnosed by a doctor by means of a digital rectal exam, an anoscopy or anal cytology.
Depending on what the warts are like, their number and location, the doctor may recommend their removal by applying a treatment with a cream, freezing them and, in some cases surgical removal.

PrEP (short for pre-exposure prophylaxis) is a HIV prevention tool. The United States healthcare authorities approved its use in 2012 after a number of studies had demonstrated its safety and efficacy. Since then, other countries around the world have followed suit to make it available to people at higher risk of infection.
PrEP is a HIV prevention strategy whereby HIV negative people take antiretroviral drugs to reduce their risk of infection. According to the research findings it is almost 100% effective in preventing HIV transmission in people who use it consistently.
Post-exposure prophylaxis (PEP) is also a HIV prevention strategy for HIV-negative people who take antiretrovirals but in this case they do so AFTER they may have been exposed to the virus.
Experts and regulating bodies such as the WHO (World Health Organisation) and the European Aids Clinical Society (EACS) recommend PrEP for sexually active people who belong to population groups that are most exposed to HIV, with gay men, bisexuals, other men who have sex with men, and transgender women at the top of the list.
Although studies are underway with other drugs, for now the only drug that has been approved for PrEP goes under the brand name of Truvada. In actual fact it is a tablet that combines two drugs: Emtriva (emtricitabine, also known as FTC) and Viread (tenofovir also known as disoproxil fumarate or TDF).
The drugs that are used for PrEP are very safe and have a low toxicity profile. The majority of people who use them have not reported side-effects and when these do appear they tend to be mild. Even so, PrEP needs a prescription and must always be taken under a specialist doctor’s supervision to guarantee safety.
For those registered in the Canary Health System (SCS), PrEP is derived from Primary Care or other community entities. The situation is very different from that of other autonomous communities in Spain and/or the rest of Europe. You need to see your GP in the first instance.
The complication is for visitors and tourists, there are no adequate facilities since the medications are not available in pharmacies, but only in hospital HIV departments or specialist units.
It is recommended that all visitors bring more than the quantity of PrEP needed for the duration of their visit in case of unforeseen circumstances.
In countries where PrEP has not been approved yet, some people decide to follow this prevention strategy by themselves either by obtaining Truvada on the black market or legally by importing generic drugs for personal use as in the case of the UK.
If you are thinking of taking PrEP on your own you need to take some precautions: make sure there are no contraindications for the drug in your particular case, check that you are not infected with HIV and take regular medical checkups.
If this is your case, at checkpoint Canarias we can offer you guidance on how to minimise any possible risks that go along with PrEP under these conditions.
Non-occupational post-exposure prophylaxis is a secondary prevention measure aimed at preventing the development of HIV infection after accidental exposure to the HIV virus through sexual intercourse.
It consists of treatment with antiretroviral drugs for 28 days, which should be started as soon as possible. It is an exceptional measure.

The only way to know if you have HIV is to get tested. Knowing your HIV status helps you make healthy decisions to prevent getting or transmitting HIV.
When people with HIV don’t get treatment, they typically progress through three stages. But HIV treatment can slow or prevent progression of the disease. With advances in HIV treatment, progression to Stage 3 (AIDS) is less common today than in the early years of HIV.
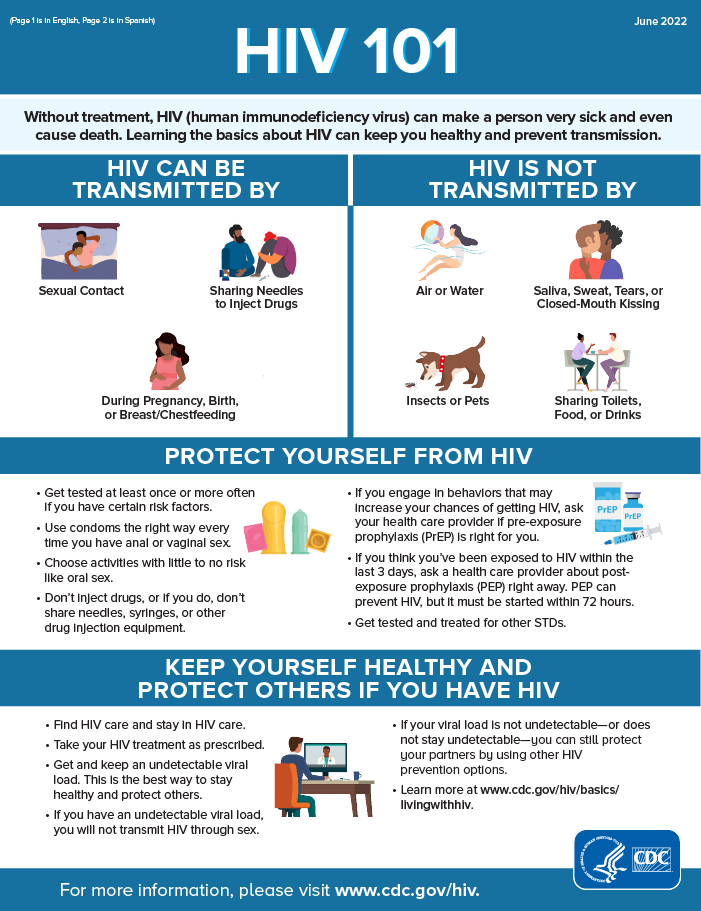
The US Centres for Disease Control (CDC) have published this informative summary leaflet
For more detailed information click here for the US CDC website.
It is the intentional use of drugs (substances) to have sex over a long period of time (from several hours to several days) among gay men, bisexual men, other men who have sex with men (MSM) and more recently, people with other identities sexual (trans women, non-binary people, queer…). Some terms that are used colloquially are: session, chill, etc.
Both at sex parties in private homes and in commercial sex venues (saunas, rental flats or sex clubs) and in cruising areas.
Consumption can be solo (for example, virtually: watching porn or chatting on live camera), one on one, threesomes or group sex (this implies that it can be between groups of friends, in open or closed relationships, with sexual partners and/or with strangers). In addition, the use of contact pages, mobile applications and WhatsApp is very frequent.
For now we’re pointing you to this website for more information in Spanish or here in English. For support in Spanish or English see our page here.
checkpoint Canarias can undertake rapid testing for the following: HIV, Hepatitis C, Syphilis, Chlamydia, Gonorrhoea.
To make an appointment at our Maspalomas clinic, click here.
In the Canary Islands there are a number of options for a full in depth screening depending on the health cover you have.
They should perform a combination of the following tests depending on your sexual orientation and sexual practices:
Photo by Julia Koblitz on Unsplash